Blog: Herding cats or Flying with the Flock? Experiences of co-designing health systems interventions to improve health in complex urban environments (ICUH Panel Session, Atlanta 2023)
With multiple stakeholders, all with competing agendas and different expectations – how do you effectively co-design sustainable, feasible, equitable interventions to strengthen health systems?
At the 19th International Conference on Urban Health, in Atlanta, USA November 2023, CHORUS researchers from all partner countries contributed to a panel session to share our lessons and findings from this process of co-designing interventions to strengthen urban health systems. The session included videos and presentations from our teams from Bangladesh, Ghana, Nepal and Nigeria to explain and reflect on the co-design process and the resulting health system adaptation. Presenters then formed a panel, moderated by Prof. Zahidul Quayyum from James P Grant School of Public Health, BRAC University, to discuss some of the challenges of the codesign process, including:
- Addressing power imbalances within health services so key voices can be heard.
- Managing expectations and prioritising interventions within resource-constrained environments
- Facilitating meaningful community engagement, considering differences by gender, occupation, education and other characteristics within each context.
CHORUS works with many city actors, to develop and test health system interventions to improve the health of the poorest urban residents. Over the past two years, CHORUS teams in cities in the four countries have conducted extensive needs assessments in each city, using a mix of household and facility surveys, qualitative and participatory methods as well as systematic and literature reviews to ensure best practice informs the codesign process and analysis of national and city data sets such as WHO’s STEPS survey and Demographic and Health Surveys to ensure the changing health needs of urban populations are fully understood.
To successfully co-design interventions with multiple stakeholders, the CHORUS teams have been diligently and purposefully building collaborations with community members, public and private health providers, city or local government officials and elected representatives over the last two years. This has involved careful ongoing engagements to develop trust and sustainable relationships to strengthen health system interventions for improved health in cities. This process ensures interventions are embedded within the existing urban health systems in which they are being developed.
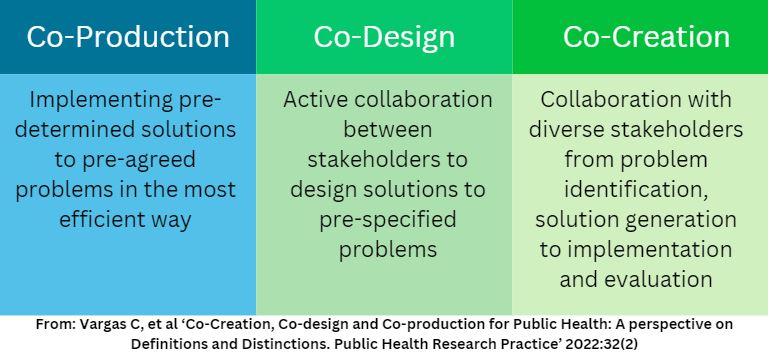
The engagement of stakeholders in the development and implementation of initiatives is recognised as the best way to ensure interventions meet the needs of local populations whilst also fitting within current systems and policy frameworks. Given the success of this way of working, there have recently been attempts in the academic literature to explore and describe different ways of working together to develop interventions. One valuable approach is put forward by Vargas et al (2022) who distinguish between co-creation, co-design and co-production (see below).
These experiences from CHORUS teams of co-designing interventions for health system strengthening, have led to three key lessons.
- Managing expectations in resource constrained systems and responding to healthcare hierarchies is a significant challenge. To manage this, teams can work with stakeholders to set priorities, and this must be done through careful consensus building. This is an iterative process and is dependent on the process being fully inclusive. Stakeholders need to maintain ownership; the process needs transparency and will be developed through trust. This level of trust needs to be built over time.
- Ensuring meaningful participation and collaboration with key stakeholders, including community members, service providers, policy makers, can strengthen the feasibility and sustainability of an intervention, ensuring it is meeting the needs of those involved, and is designed according to the context. However, ensuring engagement is meaningful, respectful and inclusive of all perspectives, whilst involving a range of stakeholders with different interests and power dynamics takes planning and deep knowledge of the context.
- Finally, the process must be conducted in a systematic way. The co-design approaches used by the CHORUS teams have frequently drawn on the useful description of the process of co-design outlined by Wight et al (2015) in their Steps for Quality Intervention Development (6SQuID) approach. While the steps may not be totally linear, CHORUS have found 6SQuiD a useful framework to plan and reflect on their co-design activities. Attempting to document the process to allow teams to draw out the key lessons is valuable, but facilitation – often by someone or some other stakeholders outside of the process – can be helpful in identifying lessons not captured in written reports.
Urban health systems are truly complex, with multiple health providers and government bodies frequently split between national and city level. The importance of the wider determinants of health in cities – such as transport, pollution and contamination, housing, access to green spaces, and more – means that there is an even wider range of stakeholders to engage with in cities. In addition, communities, particularly the poorest are frequently transient, work long hours for daily survival and therefore find it hard to engage with processes of consultation and participation. Being cognisant of all the factors, and actively identifying stakeholders that can influence and support change and bringing them on board early in the process is a key lesson learnt. While co-design may be lengthy and use more resources than more top down approaches, the ownership and trust which a good co-design process can crystallise, are key to developing effective and sustainable improvements to health systems in LMIC cities.
Health Policy Research Group, University of Nigeria: 'Linking informal and formal providers for improved primary care service coverage and quality, in informal settlements in Enugu, Nigeria
The co-design process in Nigeria brought together informal providers, such as patent-medicine vendors, traditional birth attendants and bone-setters, as well as community leaders, government primary care with multiple city and state decision-makers. When all stakeholders can come together to identify potential solutions, important nuances be identified and addressed.
https://youtu.be/eRo-fNHMeb4HERD International, Nepal: Building linkages between private pharmacies and local health system in primary health care for improve treatment of diabetes and hypertension in urban city of Nepal
Pokhara Metropolitan City and HERD International are working together to identify bottlenecks in the urban health system, and seek pathways to strengthen the system to deliver quality health services to the poor city residents. The process involves numerous stakeholders from community, institution and system levels. The extensive needs assessment identified private providers as a key health services providers in Pokhara Metropolitan City; they are working to improve engagement and linkages between the public and private sectors, to improve NCD care and data management.
https://youtu.be/1jMUbWx4euoARK Foundation, Bangladesh: Improving primary care and prevention of diabetes and hypertensions across government and NGOs in Dhaka
The co-design process worked across two ministries and city corporations as well as technical teams implementing app-based reporting systems.
https://youtu.be/nAvi02c1NfMUniversity of Ghana: Adapting a community health programme designed for rural areas, to meet the needs of urban poor communities in Accra
Community members have taken an active role in both the identification of issues and potential solutions, and through the Technical Advisory Groups, the teams have co-created a package of interventions to bring the services closer to the community members.
https://youtu.be/xQYffWfPm9I